(Dedication: To SP - may your PT tendon always be healthy and never let you down!)
A quick summary
Posterior tibial tendonitis occurs when the damage rate exceeds the healing rate. Our job is to decrease the damage rate and increase the healing rate. (Enjoy the videos and discussion, and be ready for surprises!)
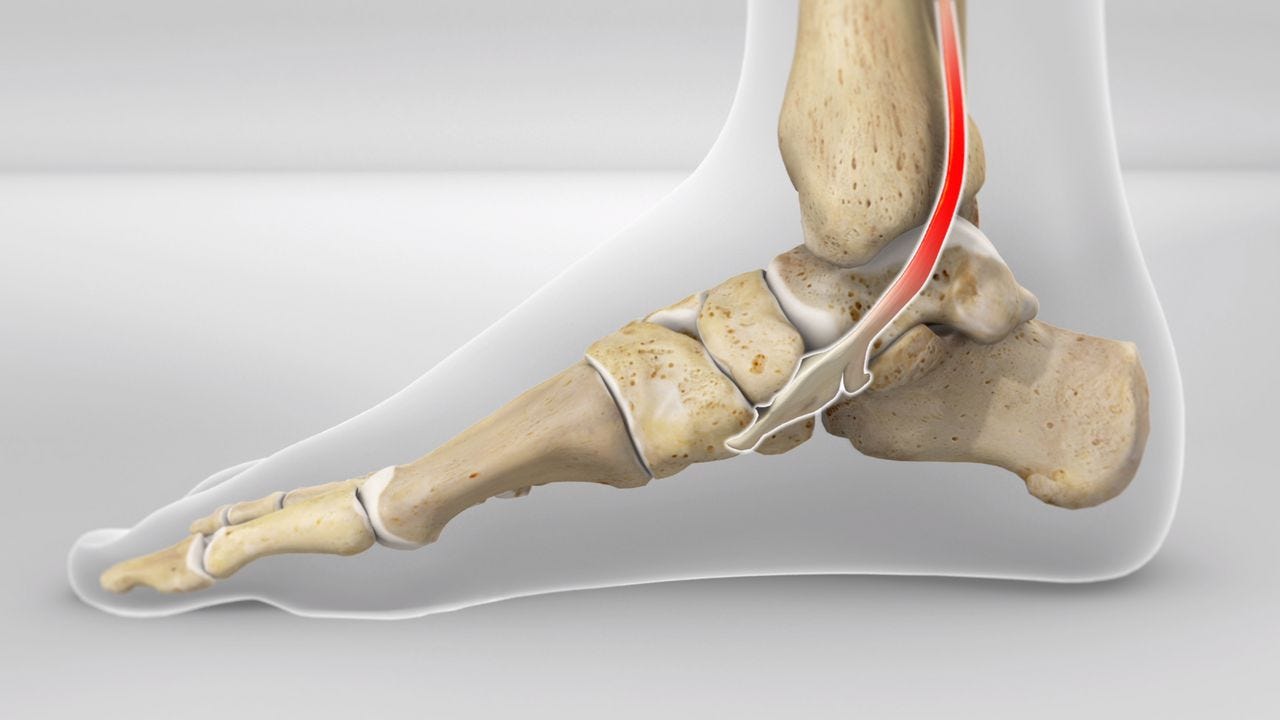
Picture: the posterior tibial tendon wraps around the back of the inner ankle bone and attaches to the foot's instep.
Video 1:
Principles of posterior tibial tendon repair & three basic exercises
After months of diligent research, I uncovered the secrets behind my exercises' effectiveness. I then dedicated additional time to producing an engaging teaching video explicitly designed so that you, too, can discover what works and why!
Video 2:
Daily exercises for posterior tibial tendonitis
I recorded this video a couple of years ago and it became Youtube hit. At the time, I knew what worked because it had worked for me and why, but I could not clearly explain the reasons.
A little bit of advertising here! All my workouts explicitly teach strong feet toes and ankles and I think this makes them rather unique (not better - just unique). Why not sign up and join me for some pilates classes online?….
Some anatomy and medical stuff
Picture: The posterior tibial tendon (PTT) starts from the PT muscle (deep to the calf muscle - not shown here) and wraps around the back of the inner ankle. The red colour indicates the area of damage. The damage occurs in the curved part of the tendon. This will be discussed further.
Posterior tibial tendonitis in stages
Stage 1 and 2: In the pictures to the left, the PT tendon is painful in the right foot which also has a noticeable loss of alignment (dropped arch, rolled-down inner ankle bone, toes pointing out to the side).
Stages 3 and 4 (shown on the right): The left foot misalignment is significant, and noticeable bony swelling and stiffness are present. Lifting the foot arch and rolling the inner ankle bone up and into alignment is no longer achievable. However, braces and orthotics, along with exercises for the sole and toe and calf and shin muscles, may still take some load off the damaged tendon, and provide some pain relief.
In the latter stages of tendonitis, due to the boney swelling, dropped foot arch, and rolled-over ankle, the tendon must turn an even longer, sharper bony corner than ever, and (as will be excpalined below) tendons are not strong when asked to do this!
Causes and solutions for posterior tibial tendonitis
So why don’t I just give you some exercises and leave you to get on with it? - The answer is because that’s what everyone else does and it’s not very effective because your PT tendon needs a lot more than “just grit your teeth and get on with it”. We’re going to show you what more you can do for your sore Posterior Tibial’s, by taking you a brief but oh so thorough discussion of causes and solutions.
(Enjoy!)
Posterior tibial tendonitis occurs when the damage rate exceeds the healing rate. Our job, therefore, is to decrease the damage rate, and increase the healing rate. Enjoy the videos and discussion (and be ready to be pleasantly surprised)
The causes (and their solutions) overlap and (a bit like a salad) can be sliced and diced and presented in different ways. In this article I’ve chosen to discuss causes under six headings. If you like this salad mix you’ll remember it and make it work for you!
(Rapid of rate of damage…)
1. Cause of increased rate of damage due to lazy foot arch muscles and rolled down ankle
2. Cause of increased rate of damage due to lack of developmental stimulus
3. Cause of increased rate of damage due to unequal loading across a sharply cornering tendon
(Slow rate of healing…)
4. Cause of slow healing: poor direct blood supply to the tendon
5. Cause of slow healing: diet and lifestyle factors
6. Cause of slow healing due to generalised high blood pressure and poor vascular health
1. Cause of increased rate of damage due to lazy foot arch muscles and a rolled down ankle
When the foot is flat and the inner ankle bone rolls down (and even more so in the later stages of posterior tibial tendonitis—examples in the pictures immediately below), the tendon must turn a sharper and longer corner, which creates tendon trauma and a loss of blood supply.
The solution to weak foot arch muscles and rolled-down ankle
The solution is to strengthen the muscles supporting the foot arch (all of them), ensuring that the posterior tibial muscle isn’t tasked with lifting the foot arch all on its own. This way, the PT tendon gets to take a relative rest so that the rate of healing can exceed the rate of injury!
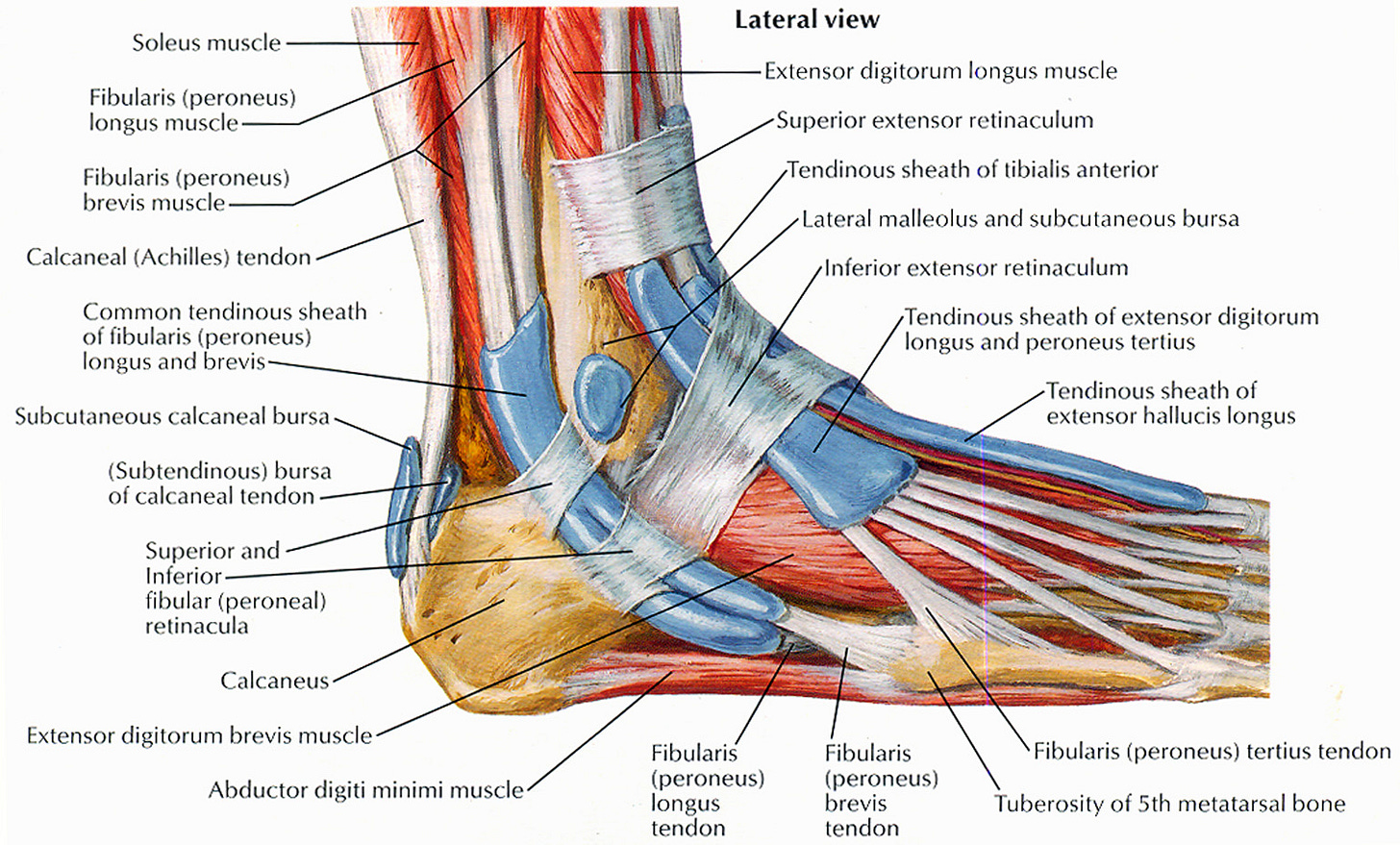
Picture: All the muscles (every one of them!) below the knee should work together to lift, shorten, narrow, and brace the foot's arch structures. However, when the team of foot arch lifters is weak and lazy, the posterior tibial is left to do all the work (not good!)
2. Cause of increased rate of damage due to lack of developmental stimulus
Suppose the toddler or child is neither active, nor bare footed on rough natural ground? - The foot and ankle muscles will not be stimulated and exercised. - In that case, they foot and ankle muscles will never fully develop and contribute to the foot arch lifting “team” - leaving the posterior tibial tendon to do all the work! – With inevitable problems in later life, and especially after the age of forty.
The solution to lack of developmental stimulus…
It’s important to commit to regular foot and ankle exercises from an early age, before any damage occurs that makes the problem harder to fix!
A little bit of advertising here! All my workouts explicitly teach strong feet toes and ankles and I think this makes them rather unique (not better - just unique). Why not sign up and join me for some pilates classes online?….
Consider becoming a free or paid subscriber
3. Cause of increased rate of damage due to unequal loading across a sharply cornering tendon
Tendons that bear loads while moving around long, sharp corners experience unequal loading across their cross-sectional area. – For example, there is more stretch - and therefore tension - over the outer curvature of the tendon. On the other hand there is significant compressive load (due to being pushed against the bone) on the inner side of the tendon. These unequal loads will lead to significantly more damage.
The solution to unequal loading across a sharply cornering tendon…
The solution is to load the tendon heavily when it is straight, and gently when it turns a sharp corner.
Pictures: The tendon on the left navigates a sharp bony corner and is unable to safely transmit a high load, whereas the tendon on the right runs straight and can be exercised safely under a high load! (Think about this the next time you are exercising a sore tibial tendon!)
4. Cause of slow healing: poor direct blood supply to the tendon
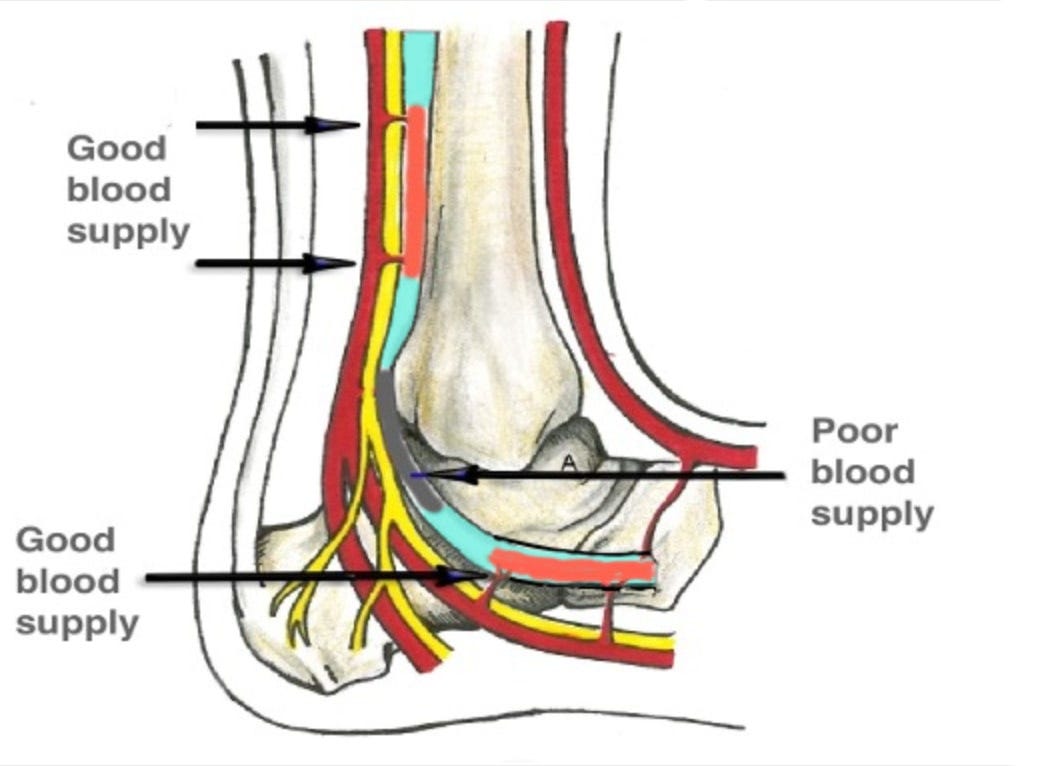
When blood vessels enter a tendon that curves around a hard, bony corner with no padding (e.g. around a dropped inner ankle bone, or when your toes are pointing up to your kneecap), the blood vessels will rub against the bone, and stretch and tear every time the tendon moves. This is why the curved part of a PT tendon has no direct blood supply and, therefore, cannot heal quickly. And (obviously) the longer the curve, the less blood supply!
Picture: the blood supply to the posterior tibial tendon (tendon is coloured turquoise) is poor in the part the tendon that “turns the corner”!
The solution to poor blood supply to the tendon…
For the blood supply to improve so that healing can occur, we must reduce the amount of curve on the tendon so that blood vessels can grow back in to more of the tendon. So…
(a) During daily activities such as walking, we can use orthotics and firm lace-up boots that support and lift the foot arch. This will reduce the extent and severity of the tendon curve. The blood vessels will then safely regenerate in the straighter tendon areas that are not now pressed hard against the bone.
(b) While exercising, we can stand on the balls of our feet to straighten the ankle and tendon. Because this will also lower the risk of damaging the tendon’s blood supply.
5. Cause of slow healing: diet and lifestyle factors
Tendons repair more slowly after age 40. Obesity, smoking, and poor diet contribute to this, as does lack of exposure to natural light (we should walk in full spectrum daylight every day - rain hail or shine).
Solutions to diet and lifestyle factors
Lose weight:-
There is a very strong correlation between obesity and tendon problems:-
(see appendix at end of article)
Avoid processed foods:-
(see appendix at end of article)
Eat organic where possible:-
(see appendix at end of article)
Healthy foods in general:-
(see appendix at end of article)
Likely useful supplements include:-
(see appendix at end of article)
Tendon toxic drugs to avoid, (if possible):-
(see appendix at end of article)
6. Cause of slow healing due to generalised high blood pressure and poor vascular health
(High blood pressure is strongly associated with Achilles tendinopathy, and therefore probably also with posterior tibial tendonitis).
The cause of high blood pressure is because the linings of the blood vessels (and the surfaces of the red blood cells) become inflamed, diseased, and, above all, sticky. This stickiness makes the blood thicker, (like treacle), so the heart must pump harder and at higher pressure, to force the blood through the blood vessels. The increased blood pressure increases the risk of rupture and bleeding of blood vessels and this just adds to the damage that blood vessels suffer when they attempt to enter a tendon that must sharply turn a bony corner. The stickiness of the red blood cells and blood vessel linings also means that the micro-circulation tends to sludge and become blocked by blood clots. The body is exceptionally good at re-routing and repairing this sort of blood vessel damage, but inevitably, there is irreversible scarring that will accumulate over the years.
The solution to generalised poor vascular health
You might want to save my blood pressure rant for another day (for example, when the doctor puts you on three different blood pressure meds but you still feel sick and tired, fat and lazy). My message is, (1) your PT tendon and sunken foot arch tissues will heal much better when they are fed and maintained by a healthy vascular system and (2), blood pressure meds never make a vascular system healthy (OK! - one exception - the Calcium channel blockers - mentioned below). They merely suppress a valuable warning symptom.
My blood pressure rant
Healthy blood cells and the internal lining of blood vessels share a common feature: both possess a glycocalyx (a glycoprotein or sugar-protein coat) that carries a negative charge. Since blood cells and blood vessels both have this negative charge, they (1) repel each other like magnets pushing apart and (2) attract a soft and slippery cushion of "exclusion zone" water around them. This means that in a healthy circulatory system, there are no crashes or traffic jams, and the flow of red blood cells resembles trains on magnetic monorails, moving friction-free. However, modern diets and lifestyles damage the glycocalyx, causing the magnetic monorail effect to stall. As a result, blood cells stick to each other and rub roughly against the blood vessels, leading to damage and sludging. Consequently, the heart must pump harder to overcome the increased friction, which is the cause of high blood pressure.
Most blood pressure medications do not enhance vascular health; they simply suppress the high blood pressure that is trying to ovecome the increased friction in the system. However, an exception might be the calcium channel blocker medications, as this class of blood pressure drugs help reduce tendinopathy.
There are well-researched natural supplements and dietary strategies that cure high blood pressure by healing and normalising the glycocalyx of the blood cells and the blood vessel walls. This topic will not be expanded in detail here but suffice to say that correcting Potassium and Magnesium deficiency (everyone on a modern diet is deficient in these), avoiding all processed foods, (no fructose and no seed or cooking oils); eating a Mediterranean diet (with olive oil and lots of greens); normalising an irritable bowel (one third or more of us have this), with probiotics and prebiotics; attention to wheat and processed milk intolerances (wheat contains weed killer that is sprayed prior to harvest to maximise the yield and milk is now an ultra-processed food; both are detrimental to health); and sensible fasting, also raw broccoli sprouts (for sulpfuraphane); kaolic garlic, and vitamin D, all help to reduce blood pressure. You should also exercise - for example everyone should walk in full spectrum daylight for a half hour every day.
My own blood pressure is 107 over 67 and I’m 65 and I’ve also healed my PT tendon. So I know what I’m talking about - The point is that blood pressure should never - except as a last resort - be suppressed with prescription drugs. But rather, we should measure our blood pressure as a guide to our Glycocalyx health.
(References must await the compiling of an article - in the mean time enjoy, or at least pardon, my rant)
Wrap up: six Pilates exercise principles that enhance the healing of the PT tendon!
(1) High loads on the tendon when it is in a straight line!
(2) Low loads on the tendon when the tendon is stretching and mobilising around a sharp corner!
(3) Exercise to achieve vibrantly strong foot and toe muscles (so that the posterior tibial muscle is not left to lift the foot arch all on its own).
(4) Strengthen the muscles of the calf, shin, and sole so that the foot arch structures bear weight smoothly during daily activities!
(5) Good ankle posture (with an appropriately lifted arch and inner ankle bone) during exercises and daily activities reduces the curve on the tendon, preventing damage and allowing it to heal (Use orthotics and listen carefully to your movement instructor).
(6) Be consistent - exercise your feet a little each day!
January 2025,
Bruce Thomson B.V.Sc.
Pilates Instructor